Health System & Hospital-Owned Specialty Pharmacy Solutions
Results-Driven Specialty Pharmacy Partner to Providers
Shields is the preferred choice for healthcare providers looking to elevate clinical care management and produce better outcomes for patients with complex or chronic conditions. Working alongside our partners, we expand payer and drug access, improve therapy management and optimize care coordination to deliver unsurpassed patient experiences and generate the net operating income health system’s need to accelerate growth.




Health System & Hospital-Owned Specialty Pharmacy Solutions
Results-Driven Specialty Pharmacy Partner to Providers
Shields is the preferred choice for healthcare providers looking to elevate clinical care management and produce better outcomes for patients with complex or chronic conditions. Working alongside our partners, we expand payer and drug access, improve therapy management and optimize care coordination to deliver unsurpassed patient experiences and generate the net operating income health system’s need to accelerate growth.
Our Nationwide Network of Health Systems
With proven success partnering with more than 80 health systems across the country and a vested interest in delivering measurable results—we are the specialty pharmacy builder and growth accelerator of choice.






Our Nationwide Network of Health Systems
With proven success partnering with more than 80 health systems across the country and a vested interest in delivering measurable results—we are the specialty pharmacy builder and growth accelerator of choice.





Our Comprehensive Offering
Leveraging the foremost leaders in the industry and an integrated care model that’s built on innovation and kindness, we work alongside our partners to accelerate the growth of their successful specialty pharmacy program.
Accreditation
Gain dual accreditation within the first 18 months, facilitating one of the many requirements for payer and drug access.
Payer Contracting
Navigate complicated payer requirements to unlock access and expand care to more patients.
Trade Relations
Facilitate market access to limited distribution specialty drugs and pipeline medications.
Implementation
Work collaboratively to define strategic goals, align resources and execute plans that drive operational excellence.
Operations
Collaborate with partners to manage a successful specialty pharmacy program. Adheres to new and existing best practices and maintains industry compliance.
340B Strategy
Work to optimize drug pricing to ensure value and expand programs and services to underserved patients.
Revenue Cycle
Support revenue collection processes to help our partners excel in specialty pharmacy growth.
The Challenge of Financial Toxicity in Cancer Care
The high out-of-pocket (OOP) costs of oral oncology agents frequently place a financial burden on patients and their families, leading patients and their families to implement coping mechanisms to manage the hardship.
- Financial toxicity is a significant risk for all patients, but especially for those with cancer.
- Patient assistance programs (PAPs) are often available to help cover the cost of oral oncology agents.
- An integrated health system specialty pharmacy (HSSP) model is best able to identify and address the risk of financial toxicity early in a patient’s treatment journey.
- Shields Health Solutions can help reduce financial toxicity in oncology care by connecting patients to PAPs; we secured $672 million in financial assistance (FA) for oncology patients in 2022.
Industry-Experienced Trade Relations Teams
Our Trade Relations experts operate side-by-side with our partner’s team to expedite access to the medications patients need while covering the following three areas with diligent research, aggregated data reporting, and compliance management:






Knowledge-Backed Payer Contracting Team
Comprised of uniquely trained specialists with profound industry experience, the Shields Payer Contracting Team works on behalf of our partners to expand network access for their specialty pharmacy programs, freeing them to focus on patient care.
Our Payer Contracting Team strategy is centered around three pillars:
Meet Access Requirements Faster
We have built a centralized infrastructure and a standardized “best-in-class” care model that can meet specialty pharmacy network access requirements across the national health insurance landscape.
Develop Customized Payer Access Roadmaps
Because no two health systems are alike, our Payer Contracting Team works with each partner to develop a customized strategy and roadmap, utilizing our proprietary data engine specific to their needs. We deploy collaboratively developed managed care tools, applying more than 50 years of managed care experience.
Sustain Clinical Compliance & Reporting
We ensure our partner health systems continually meet ever-changing payer access requirements. TelemetryRx® data insights enable partners to quickly adapt and automate critical reporting to PBMs and payers.
The Shields Care Continuum
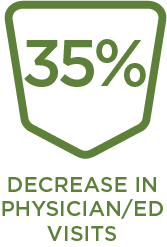
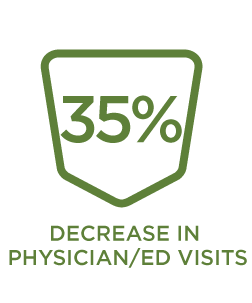
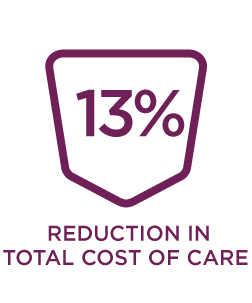
Achieving Quality Outcomes
Discover how our integrated and comprehensive offerings improve therapy management and care coordination for patients with chronic and complex diseases.
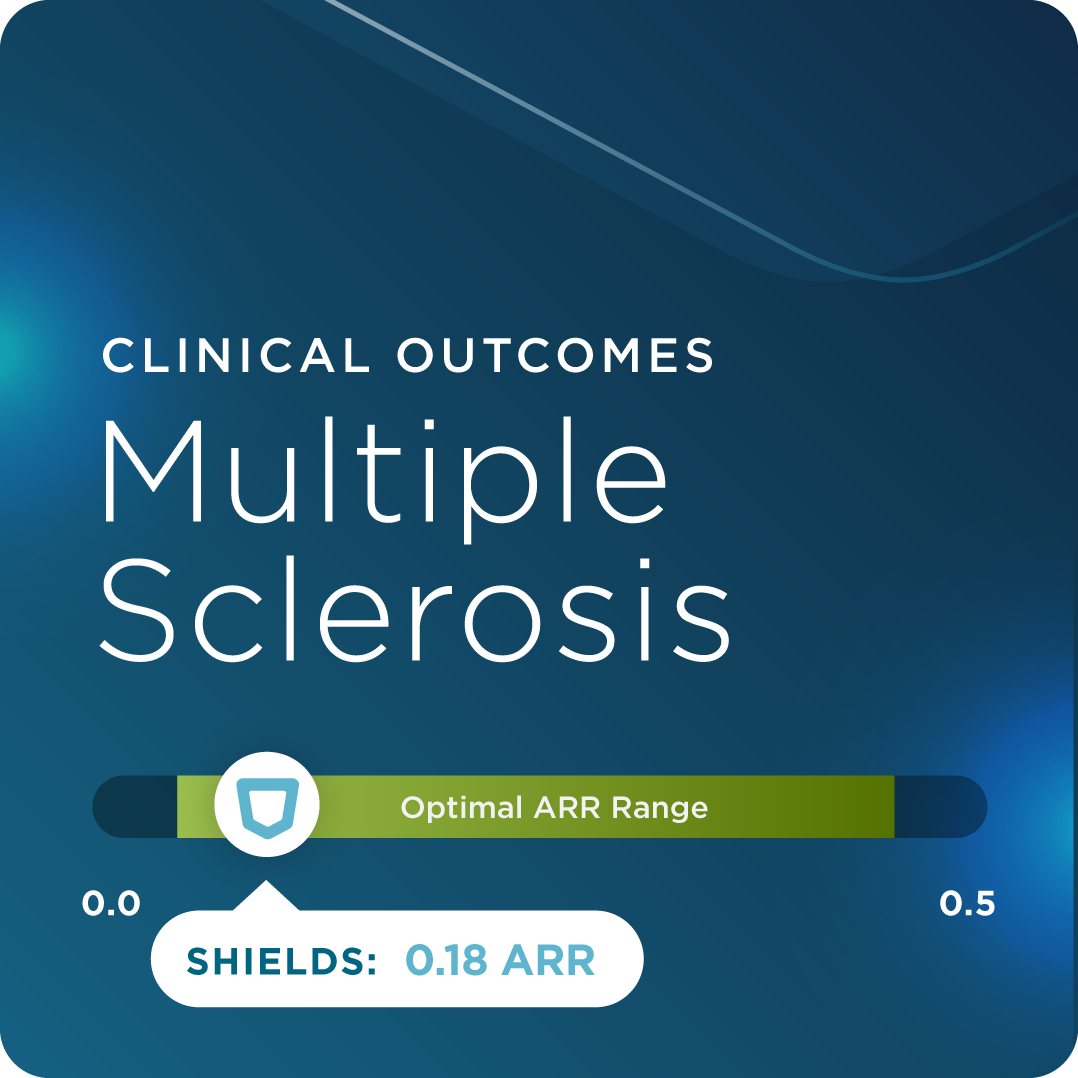
Nearly 1 million people in the U.S. live with Multiple Sclerosis. Our care model assists patients in achieving lower annualized relapse rates.
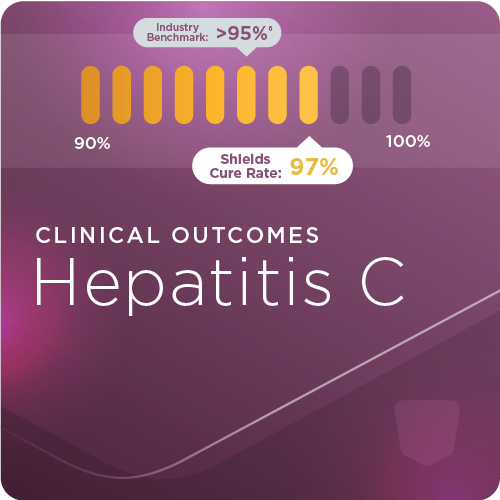
Shields Health Solutions can help patients with Hepatitis C prevent disease progression and achieve sustained viral response.
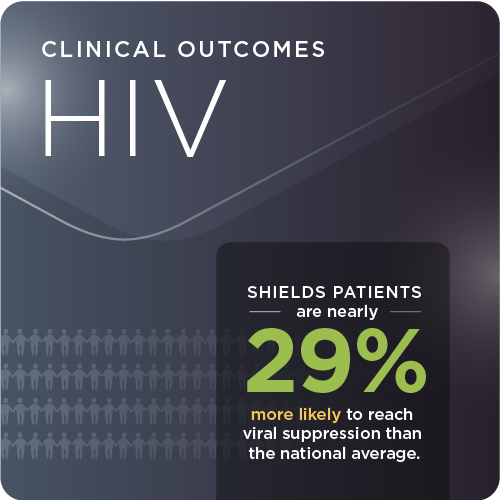
In the U.S., nearly 1.2 million patients living with HIV. Shields can help patients with access to our care model maintain viral suppression.
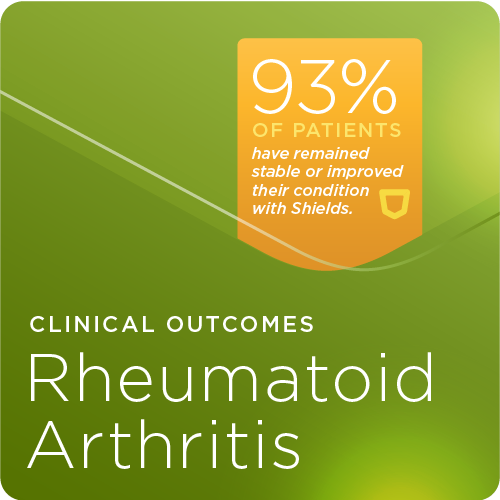
Our collaborative care model helps providers monitor this physically debilitating disease, which is vital to slowing progression.
LET’S TALK.
We’d love to hear from you.






